For a diabetic emergency, particularly when someone is experiencing either hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar), the following steps can be taken:
- Assess the Situation: Approach the person calmly and assess the situation. Determine if the person is conscious and responsive.
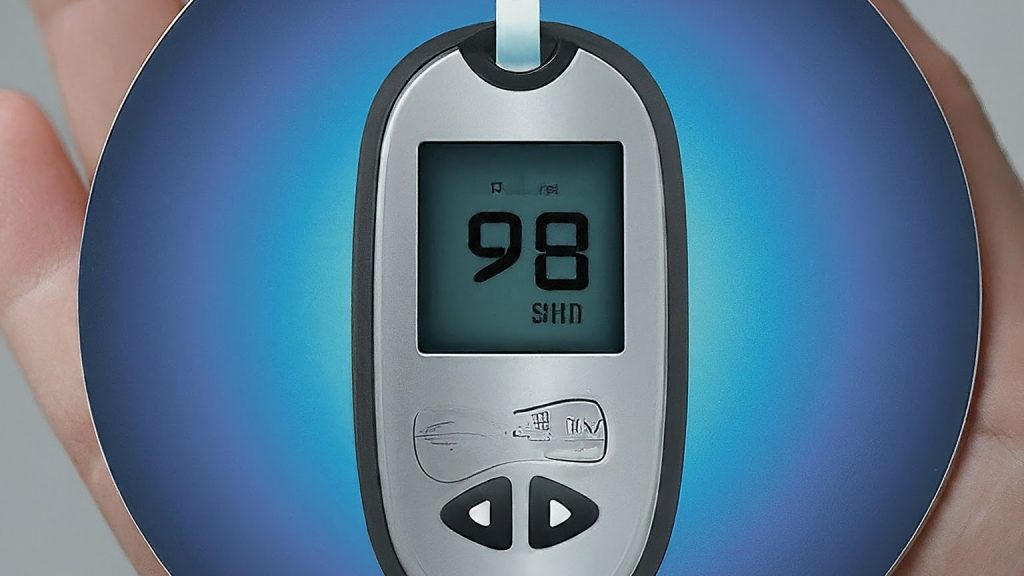
- Check Blood Sugar Levels: If the person is conscious and able to communicate, ask if they have a glucose meter and if they have checked their blood sugar levels recently. If not, and if you have access to a glucose meter, you may check their blood sugar level if they consent.
- Recognize Symptoms:
- Hypoglycemia (Low Blood Sugar): Symptoms may include confusion, dizziness, sweating, weakness, trembling, irritability, or loss of consciousness.
- Hyperglycemia (High Blood Sugar): Symptoms may include excessive thirst, frequent urination, fatigue, fruity-smelling breath, nausea, vomiting, or confusion.
- If Hypoglycemia (Low Blood Sugar):
- Give them a fast-acting carbohydrate source immediately, such as glucose tablets, fruit juice, honey, or sugar candies.
- Avoid foods with fat as they can delay the absorption of sugar.
- Recheck their blood sugar after 15 minutes. If it remains low, repeat the treatment.
- If Hyperglycemia (High Blood Sugar):
- Encourage the person to drink water to stay hydrated.
- Monitor their condition closely. If they have high blood sugar levels and exhibit symptoms of diabetic ketoacidosis (DKA), a life-threatening complication of diabetes, seek medical help immediately.
- Stay with the Person: Monitor their condition closely. If they become unconscious, call emergency services immediately.
- Seek Medical Help if Necessary: If the person’s condition doesn’t improve or if they lose consciousness, call emergency services immediately.
- Provide Support: Offer reassurance and support to the person throughout the process.
Remember, it’s crucial to act promptly and seek medical assistance if needed, especially if the person is unconscious or if their condition doesn’t improve with initial treatment. If you’re unsure about the appropriate steps to take, it’s always best to err on the side of caution and seek professional medical help. For more information, be sure to take a first aid course!